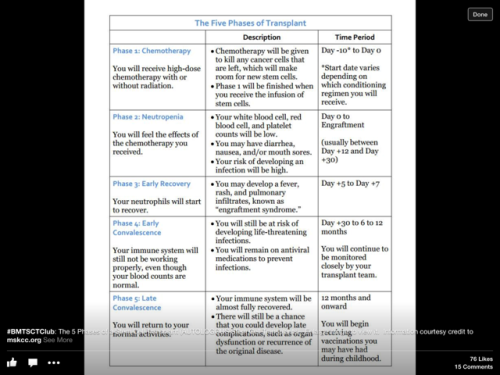
Yet again it has been so long since I last posted that I am having to play catch up. Time has passed so quickly, the exceptionally mild winter moved as swiftly as the swallows and swifts arrived into an early warm and sometimes very wet Spring, fruit trees laden with pink and white blossom and new green foliage eagerly bursting through the soil. I was in hospital the latter part of March and half way though April last year having my cord blood transplant and more or less missed out on Spring so it has been a real delight to witness it this time. However it has been extremely hard to find the energy, concentration and inclination over the last few months to update my blog. I have tried and done the odd bit at a time but now I’m just going to get an update out there whilst I’m having a steroid day! It isn’t all I wanted it to be but if I put it off any longer, it may never happen. It is somewhat a technical update about treatment which hopefully you will get through in order to understand the backdrop to my world the last few months. Life with myeloma and on treatment has been even more of a rollercoaster ride than usual. Coping with the side effects of the treatment, fatigue, chemo brain, depression and infections has taken its toll. Although it has been about 5 months since my last post, time has a different dimension for me with little to distinguish one day to the next, yet although I am doing less, it doesn’t feel like it is passing more slowly. An average day for me might consist of a hospital appointment, going shopping or an hour in the garden or a meet up with a friend or watching TV and that is all I can manage except on steroid days.
Lets start with a (fairly) brief recap…
Late December 2015
I ended the last post on a bit of a cliff hanger as I was waiting for my clinic appointment on 31 December to find out the result of the light chain test from the end of the second cycle. It was very bad news, they had risen sharply to 3600mg/l. The hope that Revlimid might have kickstarted some graft versus host disease and with that some graft versus myeloma effect or that my new cells would be resensitised to treatment were dashed. I was desperate to switch to a different treatment but there wasn’t anything left on the NHS that was available to me apart from Bendamustine, an old chemotherapy drug from the sixties which seems to have had a bit of a renaissance recently for treatment of relapsed myeloma but really is the last resort. Rather than that, the boss suggested I have a third cycle of the same treatment but increase the amount of Dexamethasone (the steroid) to 4omg x 4 days each fortnight over the 28 day cycle, an enormous dose and add Clarithromicin to the treatment regime. Clarithromicin is an antibiotic which has been shown in a recent study to overcome resistance to Revlimid, incidentally a study that I came across and informed my consultant about! In part the reason for the high dose of Dex was to try and help bring down my creatinine levels as they were elevated which was a sign that my kidney function was not good. The high dose dex might also help to keep a lid on the rising light chains as by now I was starting to feel the effects of active myeloma such as raised calcium levels, anaemia, fatigue and the reduction in kidney function. I seriously thought that I was approaching the end of my myeloma journey and that I might have about 6 to 12 months left. Note the word “left” rather than “live”. The psychotherapist on the Haematology ward whom I had been seeing didn’t try to dissuade me from my view but suggested I try and prioritise what was truely important to me if I did only have that amount of time left. What would I pack in my suitcase for 6 months, what would I leave out? What for 12 months? I found that analogy helped me put in place some plans for life rather than be waiting to die. I still haven’t packed my suitcase though!
January 2016
I started my third cycle of Revlimid, high dose dex (interestingly sex, always comes up on my predictive spelling instead of dex but I certainly wasn’t prescribed that!) and added daily Clarithromicin. A rather depressing and anxious start to 2016.
I got a high temperature about 10 days later and had to go to A&E, which is standard advice when you are a haematology patient on treatment or recovering from a transplant. After about 10 hours on a trolley in a side room there, I was transferred to a haematology ward and pumped full of IV antibiotics and fluids. I ended up staying in just under a week as I was still getting temperature spikes and the medical team were waiting for the results of swabs and blood cultures. I was given two units of blood as I was extremely anaemic and I had stage 2 acute kidney disease which used to to be called acute renal failure which is what led to my diagnosis. There is only one more stage! I had a very frank conversation with the boss on the ward round and she agreed with me that as no cause of infection could be identified and in view of my other symptoms it was more likely that it was active myeloma which was causing these problems. I was taken off Revlimid whilst in hospital as having chemo when poorly isn’t a good idea and it didn’t seem to be working anyway.
Lack of sleep, dex withdrawal, stress, anxiety and fear all played on my mind and I did think I was heading to a position where I was too ill to have any more treatment and the light chains would rise rapidly out of control ultimately in my case clogging up my kidneys and causing end stage kidney failure. After a lot of patient advocacy, I was released on parole 5 days later, the condition being I had to attend the day unit for the next few days for IV fluids, antibiotics and top ups of magnesium, phosphates and potassium. They were long tiring days but better than being stuck in hospital and my kidney function improved.
At my clinic appointment on 18 January I found out the good news that my light chains had gone down to 1300. Praise the Dexamethasone! I felt a huge sense of relief and the fear that I was approaching the “end” subsided. I started a 4th cycle of the same high dose dex regime on 26th January.
I have already described in previous posts, particularly in Dexamethasone the good the bad and the ugly just how badly I am affected by it, more the withdrawal or the crash than the actual days of taking it which just causes me to be a bit hyper and gives me some energy. It is the depression, irritability with myself and others, low mood, lack of sleep, shakiness in my voice and hands and lack of mobility due to muscle wasting that affect me so much. My physical appearance changes too, weight gain and redistribution of weight to the torso, the red moon face and hamster cheeks, humped neck, bloated stomach and hair thinning that when I see myself in the mirror I hardly recognise myself.
February
Half way through the 4th cycle when I was tested again my light chains were down to 500mg and by the end of the 4th cycle they were 344. Everyone was happy. It helped me cope with the side effects of the treatment, knowing that it was working.
March
In early March I went for a short break to Sicily with my friend and travelling companion, Jet. It was a bit of a mixed bag health wise as I had sickness and diarrhoea for some of the time and the usual fatigue. It was unseasonably cold and wet too at times but it was a change of scene and I really liked the vibrant folk art paintings of a local painter, Fiore, some of whose paintings were in our B&B but we also saw him at work in his studio. I loved the painted plastic table and chairs outside it. What a transformation of boring white plastic outdoor furniture enhanced by the bowl of Sicilian lemons!





On 26 March it was the one year anniversary of my cord blood transplant. There was nothing to celebrate about it apart from the fact of survival which is good of course, given I was given a 20% risk of mortality in the first 12 months. It was more a time to note and grieve the fact that it didn’t have the desired effect of my new immune system attacking the myeloma. I’m still not over the disappointment, but don’t know how to reach closure and let it go. Hopefully more about this in another post. I didn’t have much time to dwell on this as on 28 March I was back in hospital again for a week with a high temperature, this time with parainfluenza 3 which in immune compromised patients can develop into pneumonia. I was given the usual IV antibiotics and fluids but had to stay in until my temperature was stable and they got results back from swabs and cultures so they could see what to treat any infection with. I hate being in hospital and didn’t feel ill enough to be there which I said to the doctors on more than one occasion but other than discharge myself and risk having to go back in again with a temp spike and lose my room, I didn’t have much choice. I was taken off Revlimid again and as my light chains had gone up to 440 at the end of the 5th cycle that caused me some anxiety.
April
On the weekend after I got out of hospital I had just about recovered from the paraflu and felt well enough to travel to my parents to celebrate my Mum’s 80th birthday, then I spent the following weekend in London with a friend taking in an exhibition about Monet and the modern garden and lots of good food. It felt good to be able to do these kind of “normal” things but when I got back I felt poorly and I came down with yet another viral infection with cough and cold symptoms, this time my old foe Adenovirus. I am only just getting over this nearly 2 months later and it has really wiped me out. On 21 April I started a 7th cycle of Revlimid, Dex and Clarithromicin. Light chains were 98 at the end of the sixth cycle. That was a really spectactular drop especially as that cycle was messed up as I wasn’t on treatment for a week and a half. I was delighted and relieved but slightly anxious that it could be a lab error. Also the boss pointed out recently that I did take a double dose of dexamethasone during that cycle.
May
Despite the fatigue and the virus, May has been a quite a busy month so far. In early May, I ventured out in the evening, a rare event, to a couple of dance performances. As a birthday present from my parents, I tried out my flying skills on a flight simulator which was surprisingly realistic and fun. I landed in Hong Kong and St Maarten in the Caribbean fairly successfully without taking off too many roofs!. Then over my birthday I celebrated with friends and family with lots of meals out and cake. I also did a lovely 5 mile walk in Dovedale in the Peak District. It was all quite exhausting especially as I was steroid crashing but I’m glad I did it. I really didn’t think when I was first diagnosed at 49 in 2010 that I would make it to 55. At that time there was a 40% chance of survival for 5 years.
I started an 8th cycle of treatment on 19 May. The dex dose has been reduced from 40 to 30mg for the first 4 days of the cycle to see how that goes. The boss thought my fatigue was due to the cumulative effects of the treatment and the viral infections. I also found out the results from the 7th cycle, my light chains were up to 160 from 98. Although up a bit, I was relieved that the previous months result wasn’t likely to be a lab error as they were not far apart.
Ok that is the update done at last! I included some of the things I have managed to do as a reminder to myself that there have been some good times and productive enjoyable days, but mostly I feel like life has passing me by as the last couple of months have been really tough going, both emotionally and physically. There have been so many arrangements I have had to cancel or events that I wasn’t able to go too because I’ve been either been too tired, unwell, or just not the right mind to attend or all three. Then I berate myself for not going. I have learnt that fatigue is not about whether I sleep well or not, which I generally don’t, verging on insomnia at the moment, but like an insidious relentless brain fog. On steroid days I make all sorts of plans, have more energy and feel quite good. But in the crash period that follows all those plans go out of the window and I just try to get through the day. It means that going to weekly classes or getting involved in anything on a regular basis is really difficult to manage as I never know how I am going to be from one day to the next. My quality of life is fairly poor at the moment and that may not change as I will be on treatment for the rest of my life now. When the current treatment combo stops working as my myeloma develops resistance to it, I will switch to something else. There will be no periods of drug free remission, no more transplants, another donor transplant would be too toxic and unheard of. So my challenge remains as always to live in the moment and live as well as possible, accept my limitations, get the balance right and not give myself a hard time if I don’t always achieve it. As I like to think of myself as a pretty good card player, I find this quote very apt!
“Life is not a matter of holding good cards, but of playing a poor hand well.”
― Robert Louis Stevenson